Blood sugar control is more than just a medical term; it’s a crucial part of daily life for over 34 million Americans living with diabetes, according to the Centers for Disease Control and Prevention (CDC). If left unchecked, high blood sugar levels can lead to a myriad of health issues, including but not limited to heart disease, kidney failure, and vision loss. This sets a pressing need for effective management strategies.
The alarming fact is that failure to control blood sugar can increase your risk of developing these complications by as much as 60%. This isn’t just a concern for those already diagnosed. An additional 88 million American adults—approximately one in three—have prediabetes, a condition where blood sugar levels are higher than normal but not high enough to be categorized as diabetes.

This comprehensive guide will serve as your roadmap for effective blood sugar control, featuring expert advice, the latest scientific research, and actionable steps for immediate improvement. Whether you’re already diagnosed, at risk, or even just concerned about a loved one, the statistics and insights shared here should arm you with the knowledge to take control of your health.
Understanding Diabetes and Blood Sugar

When it comes to blood sugar control, a solid understanding of diabetes and the role of blood sugar is essential.
What is Diabetes?
Diabetes is a chronic health condition that affects how your body turns food into energy. Essentially, the food you eat gets broken down into sugar (glucose) and released into your bloodstream. In response, your pancreas produces insulin, a hormone that helps glucose get into the cells to be used for energy. People with diabetes either don’t produce enough insulin or can’t efficiently use the insulin they do make, leading to elevated levels of glucose in the blood. According to the Centers for Disease Control and Prevention, about 34.2 million people in the United States have diabetes, which underscores the critical need for effective management strategies.
The Role of Blood Sugar Level in Diabetes
Blood sugar level serves as a crucial biomarker for diabetes management. High blood sugar, known medically as hyperglycemia, can lead to severe complications like kidney failure, heart disease, and vision loss if not properly managed. Conversely, low blood sugar (hypoglycemia) can result in symptoms such as dizziness, nausea, and even unconsciousness. Monitoring your blood sugar is an integral part of diabetes management, as frequent checks can help tailor your treatment plan and alert you to any immediate issues that may need medical attention.
Ensuring your blood sugar remains within a healthy range involves a comprehensive approach, including medication, lifestyle changes, and regular check-ups. Research from the American Diabetes Association indicates that keeping blood sugar levels close to normal can prevent or delay diabetes-related complications.

By understanding the interplay between diabetes and blood sugar, you can take proactive steps to maintain a healthier, more stable life.
Types of Diabetes
Understanding the types of diabetes is crucial for effective blood sugar control. Mayo Clinic describes three primary forms of this condition: Type 1, Type 2, and Gestational Diabetes. Each type has unique characteristics and treatment options.
Type 1 Diabetes
Type 1 diabetes is an autoimmune condition where the pancreas produces little to no insulin. This type often develops in childhood or adolescence but can occur at any age. Managing Type 1 usually requires insulin therapy and regular blood sugar monitoring. According to CDC, keeping track of blood sugar levels is vital for individuals with this type.
Type 2 Diabetes
Type 2 diabetes is the most common form and usually develops in adulthood. This type occurs when the body becomes resistant to insulin or doesn’t produce enough insulin. Lifestyle changes like diet and exercise are often effective in managing this type of problem. Healthline offers a comprehensive guide on 14 Easy Ways to Lower Blood Sugar Levels Naturally, which can be particularly useful for people with Type 2 diabetes.

Gestational Diabetes
Gestational diabetes occurs during pregnancy and typically resolves after childbirth. This type can be dangerous for both mother and child if not properly managed. Mayo Clinic provides various treatment options for gestational diabetes.
For optimal blood sugar control, identifying the type of diabetes you have is the first step. Following this, tailored treatment plans can help manage symptoms and complications.
High Blood Sugar and its Consequences
High blood sugar is a condition that can have serious immediate and long-term consequences. This is especially true for those with diabetes, where blood sugar management is critical.
Symptoms of High Blood Sugar
When blood sugar levels spike, several symptoms can manifest. These can include extreme thirst, frequent urination, and blurred vision. According to WebMD, additional indicators could be fatigue, nausea, and shortness of breath. Recognizing these symptoms is crucial for taking immediate corrective actions, such as administering insulin or adjusting your diet.
Long-Term Impacts of Uncontrolled Blood Sugar
Chronic high blood sugar can lead to severe health issues down the line. The Mayo Clinic details how uncontrolled levels can result in complications like kidney disease, cardiovascular disease, and nerve damage. Moreover, consistently high sugar levels can also lead to vision problems, as cited by CDC. Long-term management often involves a combination of medications, lifestyle adjustments, and regular monitoring to prevent these dire outcomes.
Understanding both the symptoms and long-term impacts of high blood sugar is essential for anyone dealing with diabetes or at risk of developing it. Early identification of symptoms and subsequent management can mitigate the severity of its long-term effects.
Low Blood Sugar: An Overlooked Risk
While high blood sugar often steals the limelight when it comes to diabetes management, low blood sugar is an equally significant but often overlooked risk. Both immediate and long-term, the ramifications of consistently low blood sugar levels should not be underestimated.

Symptoms of Low Blood Sugar
Low blood sugar, also known as hypoglycemia, can manifest rapidly and is characterized by a variety of symptoms. Individuals may experience shaking, sweating, rapid heartbeat, and irritability. CDC adds that dizziness, confusion, and even a lack of coordination can occur. Immediate attention is essential to correct blood sugar levels through the intake of fast-acting carbohydrates, as noted by Healthline.
Dangers of Low Blood Sugar
Although often ignored, the dangers of recurrent low blood sugar episodes are significant. Mayo Clinic states that it can lead to seizures or unconsciousness in severe cases. Moreover, long-standing low blood sugar levels can also have a psychological impact, causing anxiety and fear of falling into a hypoglycemic state. Grady Health also points out that such conditions could even impair cognitive functions over time.
Being informed about the symptoms and the inherent dangers of low blood sugar can be a lifesaver, literally. It prompts timely interventions that can prevent the situation from escalating into a medical emergency.
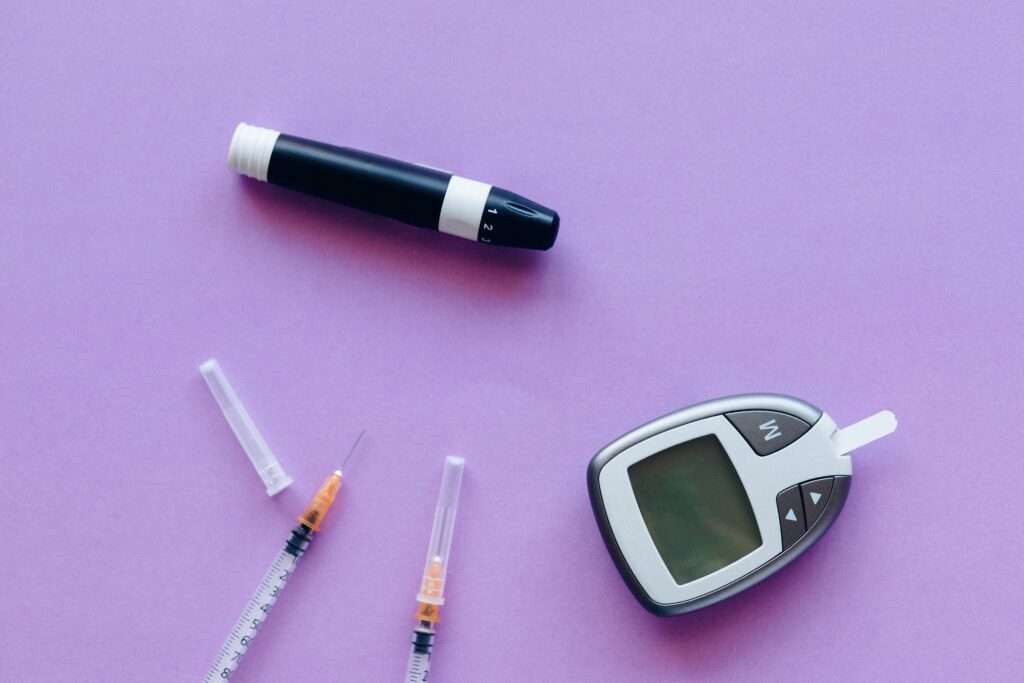
Monitoring Your Blood Sugar
In the context of diabetes management, monitoring your blood sugar is a cornerstone activity. It serves as an immediate feedback mechanism that aids in medication adjustment, lifestyle choices, and symptom management.
Blood Glucose Meters

Portable blood glucose meters are the most common tools used for at-home monitoring. These devices provide instant readings by analyzing a small drop of blood. According to WebMD, these meters are usually accurate and are increasingly being integrated with smartphone apps for easy tracking and record-keeping.
The Importance of Regular Check-Ups
Consistent monitoring through regular check-ups is essential. Even if you are vigilant with your at-home testing, professional screenings can provide a more comprehensive understanding of your blood sugar trends.
Fasting Blood Sugar Test
During routine visits to your healthcare provider, a fasting blood sugar test is typically performed. As Mayo Clinic notes, this test measures your sugar levels after an overnight fast and offers a baseline metric that can be instrumental in medication adjustments.
Check Your Blood Sugar Levels at Home
While clinic tests offer a detailed perspective, there’s merit in daily at-home checks. Healthline discusses how they allow for immediate action, helping you to adjust your insulin doses or diet in real-time, thereby aiding in more effective diabetes management.
Regular monitoring serves as a proactive measure in managing the unpredictability associated with fluctuating blood sugar levels. Through a combination of at-home and professional testing, individuals can maintain a balanced approach to diabetes care.
Natural Ways to Lower Blood Sugar Levels
Lowering blood sugar levels doesn’t always have to involve medication. Many people are turning towards natural remedies and techniques to manage their diabetes symptoms more holistically.

Herbs and Supplements
Herbs and dietary supplements can be valuable allies in the fight against elevated blood sugar levels. For example, cinnamon has been found to improve insulin sensitivity, helping your body better regulate glucose levels. According to Healthline, fenugreek seeds and berberine are other potent herbs and supplements that have shown promising results in reducing blood sugar levels. However, always consult your healthcare provider before introducing new supplements into your regimen.
Mindfulness and Stress Reduction
Besides dietary considerations, lowering your stress can also significantly influence your blood sugar levels. Techniques like meditation, deep-breathing exercises, and mindfulness can help keep you calm, thereby lowering the hormone cortisol, which in turn can improve your blood sugar control.
How Stress Affects Your Blood Sugar
Stress directly impacts your blood sugar levels by triggering the release of stress hormones that cause your body to release stored glucose into the bloodstream. As explained by the Mayo Clinic, stress management techniques can be as effective as medication when it comes to reducing blood glucose levels.
By incorporating herbs, supplements, and stress management practices into your daily routine, you can take a more natural approach to lower your blood sugar levels. It’s always crucial to consult your healthcare provider when making such changes, especially if you’re already on medication for diabetes.
Diabetes Management Plan
Managing diabetes effectively requires more than just medication; it calls for a comprehensive Diabetes Management Plan that tackles the disease from multiple fronts.
How to Create a Customized Plan
Creating a customized Diabetes Management Plan begins with a deep understanding of your specific condition. It should involve monitoring your blood sugar levels, understanding your triggers, and recognizing how lifestyle choices impact your condition. Start by determining your goals in consultation with your healthcare provider. Some common elements to consider include nutritional planning, exercise regimens, and medication schedules. According to the CDC, even a small change like reducing portion sizes can significantly improve blood sugar control. Make sure to regularly review and adjust the plan as necessary to maintain optimal health.
Role of Healthcare Providers
Healthcare providers play an essential role in formulating and monitoring your Diabetes Management Plan. They can perform necessary tests, suggest suitable medications, and provide valuable insights into how to better manage your symptoms. The Mayo Clinic emphasizes the importance of a team approach to diabetes management. This team often includes doctors, nurses, dietitians, and even mental health professionals.
With a customized plan and a strong healthcare team, you can take control of your diabetes rather than letting it control you. It’s vital to maintain open lines of communication with your healthcare providers, as regular feedback allows for the timely tweaking of your plan. Remember, proper diabetes management is a long-term commitment that demands a strategic approach tailored to your specific needs.
Conclusion

Wrapping things up, this guide has aimed to provide a comprehensive look at various facets of managing and controlling blood sugar levels.
Summary of Key Points
We’ve delved into creating a Diabetes Management Plan that focuses on nutrition, medication, and the critical role of healthcare providers. You’ve learned how a personalized plan can go a long way in helping you maintain a healthier lifestyle. The plan should be an evolving document, regularly updated based on results and feedback, as suggested by the CDC. The importance of a multidisciplinary healthcare team, as highlighted by the Mayo Clinic, cannot be overstated either.
Take Control of Your Blood Sugar Today
The data and advice available are abundant, but ultimately, the responsibility for managing your blood sugar falls on you. It’s time to take control of your blood sugar today. Harness the knowledge and resources around you, such as easy-to-follow suggestions from Healthline on lowering blood sugar naturally. Consistent and informed actions can dramatically improve your quality of life.
The ball is in your court now. Whether it’s adopting a new diet, starting an exercise regimen, or building a healthcare team, the steps to controlling your blood sugar are within your grasp.
We have compiled some of our top articles for your reading pleasure. Take a look at them whenever you have the time.